by Cassandra Stafford, MS, CCC-SLP/L, ATP (Speech-Language Pathologist and Assistive Technology Professional), NWACS Board Member
The idea of conducting an augmentative-alternative communication (AAC) evaluation for an adolescent or adult with intellectual/developmental disabilities (IDD) can feel daunting. Most SLPs haven’t done many (if any) – and it somehow feels like it should be “different” from what we do for children with complex communication needs. In reality, we still use what we know about language development and we still look to identify the person’s communication needs and the tools that may be a good fit for them.
The elephant in the room here is funding. How the evaluation, and by extension, the recommended communication system, are being paid for will directly impact the number of sessions/amount of time available to conduct the full evaluation. To the extent possible, here is my general approach to assessing adolescents and adults with IDD for AAC.
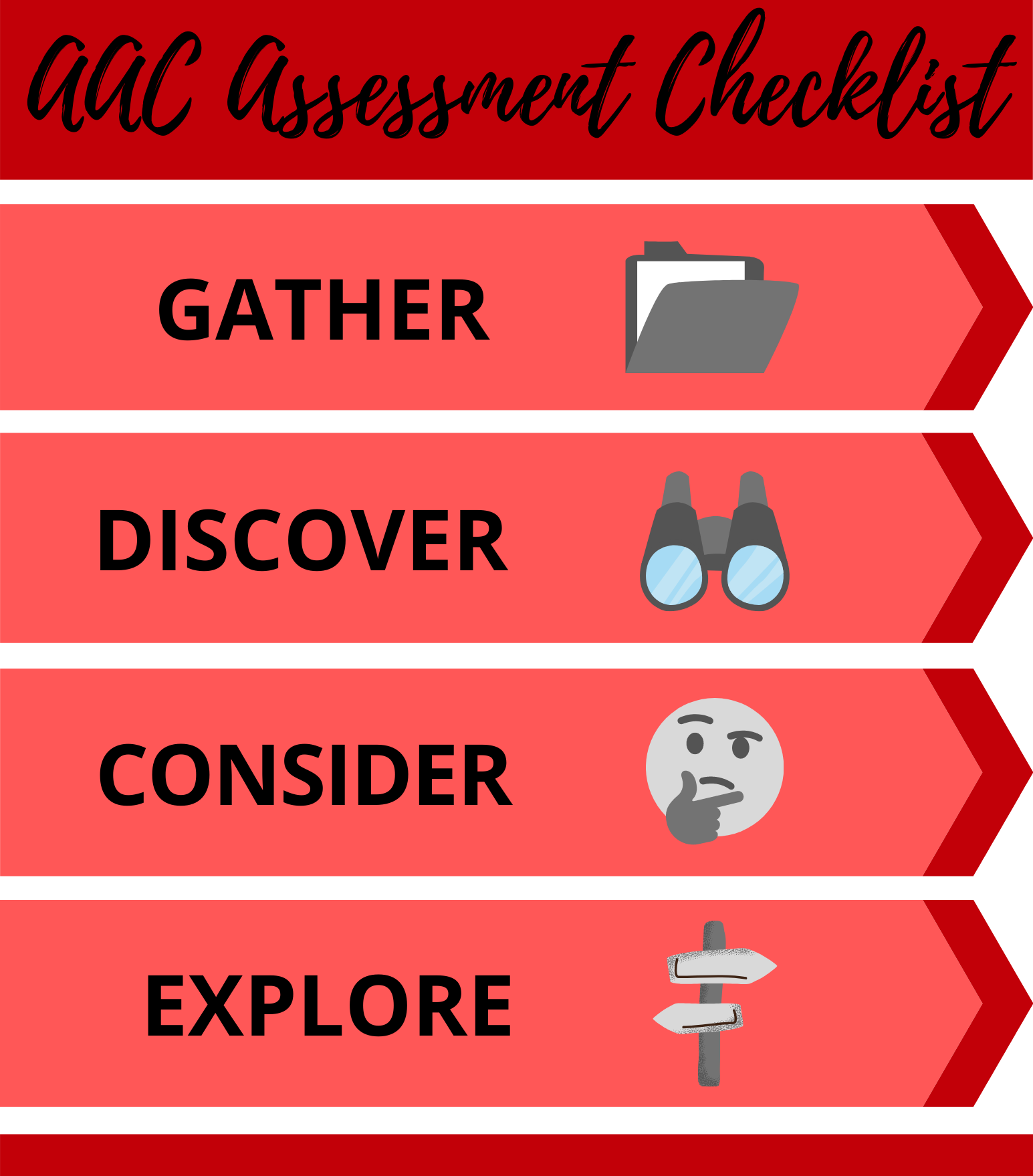
GATHER
My first step is always gathering information about the individual.
If I can, I try to ask for records to review prior to the first appointment. If the individual has a DDA case manager, I ask for their most recent assessment which contains good background information, including diagnoses, medications, and current skills and needs in many areas. If the individual is still in school, I ask for their most recent three year evaluation and most recent IEP. Additional sources for records include from other providers (OT, PT, audiologist, vision specialist, behavior specialist, etc.) and the programs they attend. Sometimes I get a good amount of records to review, and sometimes I need to rely solely on what I can gather through other means.
My first appointment is usually focused on family and/or staff interview. Whether in person or via telephone (or telemedicine), this step is crucial. The ultimate success of any AAC system is going to be largely dependent upon caregivers and other team members buying-into and actively supporting it. The more team members I have access to, the better. The more involvement they all have from the beginning, the better! I need to hear from them:
What concerns do they want addressed?
What do they think the client needs?
What are they experiencing as communication difficulties or breakdowns with the individual?
What have they found that works? Doesn’t work?
What limitations do we have to work within (e.g., policies/rules of their group home, issues with housemates, etc.)?
What do they think and know about AAC?
I end the interview segment by giving them a few questionnaires to be completed and returned to me. These questionnaires are designed to help me gather baseline information about the individual’s daily functional communication, and may include:
the Communication Matrix or the DAGG-2
Note: depending on the team, these may also be completed via interview
DISCOVER
My focus now shifts to the individual directly. Assume nothing, question everything.
To the extent possible, I observe the individual. More than once if possible, and with various communication partners, and in various contexts if possible. As I observe and filter through information obtained in the GATHER phase, I start considering possible tools for direct assessment. I always consider standardized assessments (such as the OWLS-II, PPVT, EVT, early literacy tests), if not the expressive portions, possibly the receptive portions to delve deeper into language skills. For more verbal, but highly unintelligible individuals, I consider giving an articulation/speech assessment. When considering standardized assessments, I always reflect on what I hope to gain from it. Is the information gathered likely to shed new light on speech and/or language skills that adds to what will be obtained through interview, observation, and informal/non-standardized measures? Is standardized assessment required by the funding source?
When possible, I usually attempt the AAC Evaluation Genie. This non-standardized tool gives me the opportunity to see how the individual interacts with a touchscreen, provides some information regarding visual discrimination and identification, optimal button and field size, as well as some insights into their language and literacy skills. I consider other informal/non-standardized tools as well, such as the AAC Profile, The Functional Communication Profile, and Social Networks Inventory, among others.
For individuals who have even minimal verbal communication attempts, I ask the team to choose a period of time to write down all of the spontaneous communication from the individual for a language sample that I can then later analyze using the QUAD Profile.
If the individual has no mouth words, I may ask the team to start writing down an inventory of behaviors, gestures, noises, etc. that the individual uses to communicate (and what they think they mean) to compile a Communication Dictionary/Inventory.
CONSIDER
Now it is time to compile all of the information GATHERed and DISCOVERed.
I consider what type of communicator this individual presents as: pre-symbolic or symbolic? Unconventional or conventional? Emerging, context-dependent, or independent? These “communication categories” drive the next steps and choices – not the individual’s chronological age or perceived cognitive skills.
I consider what features in an AAC system are needed to help the individual move toward more conventional forms of communication, more symbolic forms of communication, and more communicative independence. In this video on Seattle Children’s YouTube channel (AAC Assessment Strategies for Direct Selectors: Probing AAC in the context of speech language evaluations and therapy), Marci Revelli (SLP and NWACS Board Member) uses this great analogy for thinking about “feature matching”: when shopping for a new car, you have a list of things you want in your new car. Maybe you need an automatic transmission because you don’t know how to drive a “stick”. Maybe you need something with room in the back for equipment you transport frequently. It also needs to have enough seats to fit your partner and kids. Oh, and you prefer all-wheel drive because you frequently drive over mountain passes during the winter. Armed with your list of “must-have” features, you head out to the dealerships in search of options to test drive and consider. Feature matching in AAC is similar. We sift through all our information and data collected to make a list of needed features that we then carry with us as we start looking at different AAC options to trial and consider.
If access issues have been identified, then it is time to start considering alternative access methods (such as switches, eye gaze, partner-assisted scanning) and/or supports (such as keyguards). If possible, connect with the individual’s OT and/or PT to collaborate on positioning and access options.
EXPLORE
Through the feature matching process while CONSIDERing all of the information we GATHERed and DISCOVERed, we will likely have more than one AAC option that meets our list of “must haves” and are now potential options to “test-drive”.
For those with iPad communication apps on the list to trial: I have a couple of OLD iPads that I use as loaner devices. I have several robust communication apps loaded on them. After a loan agreement is signed, I loan the iPad (“locked down” as much as I can) to the family/team for a period of time so they can explore, compare, and expose the individual to the different communication app options.
For those with light-tech (i.e., paper-based) options to consider: I will usually make these options.
For those with mid- or high-tech options to consider that I don’t have: reaching out to your vendor representatives and your state (and/or other local) lending libraries is the way forward. In Washington State, two lending libraries to consider: WATAP and SETC (Note: SETC is only for schools in WA). I do have an old BIGmack voice output device and an old Tech/Talk (8 location with levels) voice output device to trial that can help give an idea about mid-tech solutions that might work for the individual as part of an overall communication system.
At this point I am only showing the team options that meet all of the individual’s needs. So now I am more interested in what the family/team feels most comfortable with – as well as taking note of any observed preferences from the individual. If the individual is able to communicate exactly which one they want, and it meets their needs/all the parameters we have to meet, then that will most likely be my recommendation. Otherwise, what the family/team feels most comfortable supporting, again assuming it meets all of the required parameters, is what I will most likely recommend. We know that implementing AAC will most likely succeed if the communication partners buy-in and feel able to support it. I want to set the team and the individual up for the most success possible!
RECOMMEND
After “test driving” various options (and having considered at least three), it’s time to zero in on which AAC system to move forward on! Once decisions have been made regarding an appropriate AAC system (including needed accessories, such as protective case, keyguard, external speaker, etc.), then we are shifting out of the evaluation process into the recommending, obtaining, and implementing phases.
While this is my general plan as I approach an AAC evaluation for an adolescent or adult with IDD, it is important to remember that curveballs and unexpected challenges can pop up at any point in the process. Remaining flexible, being open to compromise, and being ready to pivot or think outside of the box are also important “tools” in your evaluation toolbox.
Do you provide AAC assessments for adolescents and adults with IDD? What suggestions do you have to add? Please share your thoughts (or questions) below in comments or on the NWACS Facebook page!
Related articles: